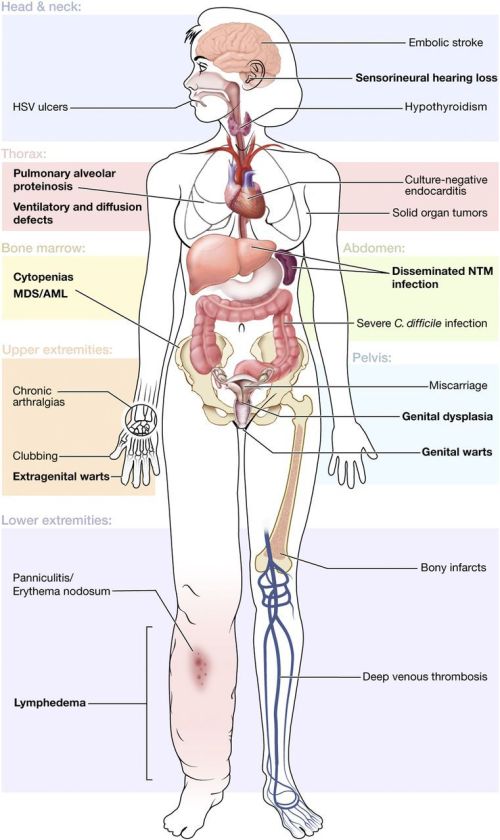
The diagram below shows all the known possible clinical features of GATA2 deficiency by organ system. Primary disease features are indicated in bold.
This page is for anyone who wants to understand more about the effects of GATA2 deficiencies. Click here to navigate to a Facebook online confidential support group for parents/carers and patients who are directly affected by a GATA2 genetic mutation.
This pool of information is a “work in progress”. I plan to update it as new research is published and/or I come across online articles that shed useful light on this topic. Links to blogs and “human interest” stories will also be considered for inclusion, if they are relevant to the topic of a GATA2 deficiency.
Please feel free to make suggestions re articles for inclusion, in the comments section below.
Leah’s myelodysplasia and monosomy 7 were caused by a mutation of her GATA2 gene. Technically, this was described as c.1061C>T or p.Thr354Met and was due to a change in a single building block of her DNA, which results in replacement of one amino acid in the GATA2 protein with a different amino acid.
GATA2 genetic mutations were only discovered in the latter half of 2011. Information about all the possible consequences of these genetic mutations was in it’s infancy when Leah was diagnosed in 2013. Click here to read an online article, published in September 2011, announcing the discovery of GATA2 genetic mutations and their link to AML and MDS.
Leah had multiple plantar warts on both feet for seven years prior to her diagnosis. We had tried many and varied treatments to eradicate these. She regularly attended a “wart clinic” run by the GP at our local Health Centre, but none of the many treatments that we tried ever succeeded in eradicating them. We now know that this problem can be associated with a GATA2 deficiency. Leah’s verrucas disappeared spontaneously a few weeks after her bone marrow transplant. Obviously verrucas on their own are not serious – it was the combination of Leah’s verrucas with her other symptoms that was the significant factor.
When Leah’s lymphocyte subsets were analysed after her myelodysplasia diagnosis, she was found to have low levels of natural killer cells (less than 1%), relatively low B cells (4%) and very low numbers of dendritic cells. This was caused by her GATA2 deficiency.
Leah went to her GP in the first instance because of menorrhagia and also because of acne on her face, neck and back, that wasn’t responding to topical treatments. The menorrhagia continued to be a problem during transplant, despite double the usual dose of norethisterone. Her GATA2 deficiency is believed to have been responsible for this. The acne required several weeks of oral antibiotics prior to transplant, to clear it.
This first GP appointment was on Leah’s 15th birthday – the 31st December 2012.
Prior to this in November 2012 Leah had several painful mouth ulcers that were difficult to get rid of and necessitated more than one trip to the chemist for an “over the counter” treatment.
At the beginning of December 2012 Leah took the really bad flu that was going round that year. She hated missing school, but she felt so incredibly unwell that she had no choice but to take a few days off school. Her energy levels were slow in recovering and she told us about sinking to her knees at school one day when her legs wouldn’t hold her up. However, she insisted that a GP appointment could not be made until the Christmas holidays as she did not want to take any more time off school.
When Leah had that first blood test on the 31st December 2012 her haemoglobin was 10.6 g/dl, platelets 123 e9/l and neutrophils 0.35 e9/I, white cell count 2.08 e9/l. There was also a lot of elliptocytes and some other abnormalities in her blood.
Leah was immediately referred to the adult haematology department of our local hospital. She commenced having weekly blood tests and had some other investigations also. Leah’s haemoglobin remained stable but her platelet count gradually decreased. Her neutrophils remained approximately the same, with some fluctuations up and down.
On the 22nd February 2013 Leah was diagnosed with acute appendicitis – this was confirmed by ultrasound, prior to surgery. Her pre-op blood counts were: haemoglobin 10, platelets 95, and neutrophils 3.36. Surgery was relatively straightforward, no transfusions were required and she made a relatively uncomplicated recovery. The surgeon did tell me however, that he had operated just in time, as her appendix was on the brink of perforating.
On Sunday the 3rd March, Leah attended the hospital as her wound was bleeding. A pressure dressing was applied. Her blood counts were then Hb 10.6, platelets 144, neutrophils 0.53, WCC 1.58. Leah returned to school full time the next day via Ulsterbus.
During all of this time, Leah had open access to our local adult Haematology/Oncology Ward and we were advised to continue with an attitude of “watchful normalisation” i.e. keeping Leah’s life completely normal, but bringing her to the hospital, or phoning the 24hr Oncology/Haematology helpline, at the first signs of any illness. I think that this was good advice as it preserved Leah’s mental health, although it didn’t do much for us, her parents! Leah got to live the “normal” bit and my husband and I got to live the “watchful” bit. Every cough, every sneeze, every tiny lump or bump, every transient ache or pain, caused my throat to tighten and my stomach to go into a knot, while outwardly I did my best to look calm and relatively unconcerned.
The next time that Leah took a day off school was on Monday 25th March 2013 when she had her first bone marrow biopsy at the Royal Belfast Hospital for Sick Children. I did not go with her, her dad and aunts did. I had never set foot in a Paediatric Oncology/Haematology Unit and I wanted to keep it that way. I love children, I work with children and I couldn’t bear the thought of seeing them so ill.
We then did not hear another word, until a doctor we had never met, or even heard tell of, phoned us on Friday afternoon 19th April and said that Leah had myelodysplasia and that she needed a bone marrow transplant. I write about this very traumatic phone call here.
We had our first outpatients appointment at the adult Oncology/Haematology Department in Belfast City Hospital on Tuesday 23rd April 2013. On that occasion, Leah’s blood counts were Hb 11, platelets 91, neutrophils 0.54, WCC 2.49. This doctor informed us that Leah also had monosomy 7, an acquired chromosomal abnormality. My husband and I found this first appointment very harrowing, we left feeling that it wasn’t just a bone marrow transplant that Leah needed, it was a miracle. I write a bit about this here.
Leah’s teenage brother was found to be a 10/10 match for donating his bone marrow to her. Leah was referred to Bristol Children’s Hospital for her treatment. Click here to read about the intense sibling rivalry that had previously existed between Leah and Simon and the words that she used to inform him that he was her compatible donor.

On the 14th June 2013 we had our first outpatient appointment in Bristol. This was the first time we heard that there was such a thing as GATA2 genetic defects. It was also the first time since we had started taking Leah to haematology appointments in January 2013 that anyone asked her if she had warts. The dots were starting to be joined. I write in more detail about our reaction to that first appointment here and here.
On Thursday 27th June 2013 our consultant in Bristol phoned us to say that they had completed Leah’s gene sequencing and they had found a GATA2 mutation. I found this news terribly distressing and I write about how I coped here.
Leah was admitted to the Bone Marrow Transplant Unit in Bristol on Monday 22nd July 2013. On arrival she wasn’t feeling well. She very quickly became seriously ill with a line infection caused by several gram negative bacteria, most notably serratia. This infection did not respond to intravenous antibiotics and her Hickman central line had to be removed. It was replaced once her infection cleared. As you can imagine, this was all very stressful, I go into more detail here.
Leah received her bone marrow transplant on the 1st August 2013.

Early in September, Leah developed cutaneous (skin) GVHD. This was graded 2/3 in severity and the diagnosis was confirmed by skin biopsy. Her rash was accompanied by very severe joint/bone pains, relieved by tramadol. Her GVHD was treated with prednisolone 2mg/kg/day along with MMF and three doses of methotrexate. I write more about this here.
In October Leah developed severe haemorrhagic cystitis. She found this the most difficult month of all. I write about our experiences with this here.
Then she developed a line related thrombosis. To read more about this event click here.
Our consultant now believes that the severity of Leah’s haemorrhagic cystitis and her thrombosis were both due to the effects of her GATA2 deficiency.
Leah was gradually weaned off her oral steroids, she received her last dose on the 22nd November 2013.
By December 2013 Leah had very severe back pain that was causing her considerable distress and curtailing her independance. She was found to have developed a wedge compression fragility fracture between T6 and T8 in her spine. There is a strong suspicion that the action of her GATA2 deficiency made her more susceptible to the side effects of steroids. Despite the pain, Leah tried to remain positive and listed all the things she was thankful for.

On Friday 27th December Leah started vomitting profusely while we were driving the seventy miles to our weekly outpatients appointment at Belfast City Hospital. While we were waiting to be seen by the doctor I noticed that she was breathing at a rate of 40 respirations per minute. I write about this appointment here.
Leah was sent for a chest x ray followed by an emergency CT scan of her chest. Then she was admitted to a single ensuite room in The Cancer Centre. I was worried and scared and I write about this here.
Leah’s medical condition deteriorated very quickly and the next day she was transferred to ICU. On the 2nd January 2014, two days after her sixteenth birthday, Leah needed a ventilator to help her breathe, due to respiratory failure. On the 16th January Leah was transferred to the N.I. Children’s Hospice, where she died in peace and dignity, surrounded by love.
I was initially told that Leah would die in ICU – to read how a transfer to the N.I.Children’s Hospice became possible, click here.
Leah’s cause of death was a rare complication of transplant, known as idiopathic pneumonia syndrome. It is thought that Leah’s GATA2 deficiency may also have played a part in her susceptibility to developing IPS.
Of course, most people won’t have all the GATA2 related problems that Leah had. It’s very unpredictable in how it affects people. Some people have very few symptoms.
Another problem that Leah had during her illness, was that anytime that she had a peripheral cannula inserted in her arm, she was very prone to developing phlebitis. Phlebitis is inflammation of the vein and can be very painful.
Generally, about three to five days after having a peripheral cannula inserted, Leah – who normally had a high pain threshold – would start complaining of pain at the cannula site. The nurses would inspect the site and there would be no visible redness or swelling so they would refuse to remove the cannula.
My daughter however, would become increasingly distressed, while I searched for a nurse who would listen to us and take this situation seriously enough to remove and re-site the cannula. It was very difficult to locate a vein on Leah’s arms so the nurses were always very reluctant and I had to be very persistent.
Eventually the tell-tale red line of inflammation would show on Leah’s arm and then she would need treatment to reduce the pain and swelling. It could take up to five days for this to completely heal.
When we returned from Bristol, our Haematology Consultant in Belfast was keen to discuss removing Leah’s Hickman Central Line, as Leah had developed a blood clot (catheter associated thrombosis) and was on daily anticoagulant injections. Leah pleaded for it to remain in place, as the hospital staff still required weekly venous access. Thankfully it was still in place when she became critically ill, although it was replaced while she was in ICU.
The GATA2 gene is believed to play a significant part in the formation of blood vessels so I assume that Leah’s susceptibility to phlebitis was yet another symptom of her GATA2 deficiency, however I have not confirmed this with any of the professionals.
Incidentally and nobody has ever suggested that this had anything whatsoever to do with Leah’s GATA2 deficiency, but when Leah was two and a half years old, she attended a routine checkup with our Health Visitor. This Health Visitor was very vigilant and noticed that Leah was unusually pale and lethargic. She arranged for Leah to have her blood checked there and then. My G.P. phoned me later that day to tell me that Leah’s haemoglobin was only 7.3 g/dl. Leah was referred to the paediatrician at our local hospital where she had some routine investigations but nothing abnormal was found. She was treated with oral iron (fersamal) and her haemoglobin gradually rose to 11.9 g/dl.
Click here for a short article that explains GATA2 deficiencies.
For more detailed information on the effects of GATA2 read GATA2_Deficiency_GD_Sept_14
If you are very medically minded you could even read this article.
Click on this link to read about the five year research programme that began in the UK in April 2015 that aims to uncover the cause(s) of familial myeloid leukaemia and myelodysplastic syndrome. Read about my meeting with the researchers here.
Click here to read a research article, published in March 2016 by the American Society of Hematology, that studied the prevalence of GATA2 mutations in children and adolescents with myelodysplasia. They found that overall, only 7% of children/young people with primary paediatric MDS have a germline GATA2 mutation. However, they found that the majority (72%) of adolescents with MDS and monosomy 7 carry an underlying GATA2 deficiency. This study also concluded that overall survival was not affected by the presence or absence of a GATA2 mutation.
Becky is a young woman living in the UK who has been diagnosed with a GATA2 mutation. Her blog is called Beckys Stem Cell Transplant.
For anyone who is really keen, this is a one hour lecture that explains in detail about GATA2 deficiency. Personally I found the lecturer quite easy to listen to and his content interesting:


Hi there,
I am sorry to hear about Leah. I am going through similar situation.
I lost my husband in July and still trying to understand the cause. The Genetics doctor gave me a call today and told that GATA 2 mutation has been found in my husband’s blood sample. My husband was diagnosed for MDS. An unrelated cord blood cell donor was found but we didnot didnot even get the chance of treatment.
The medical reason of my husband’s death is recorded as multiple organ failure due to e-coli bacterial infection. None of the anti-biotic was responding and he was declared dead 2ithin 24 hours of his admission in ICU.
Not sure what was Leah age, my husband was 30 and he lost his siblings due to unidentified reasons and all the doctors suspect that the GATA2 mutation is running in the family. I read through the GATA2
I just want to say “THANK YOU VERY MUCH” for writing the blog.
LikeLiked by 1 person
I am so very sorry to hear of your husband’s death, it sounds like everything happened rather quickly and that his death was most unexpected. I know that you must be feeling very raw and very devastated as you try to make sense of everything that has happened. If there is any way that I can help, please let me know. ❤️
LikeLike
I have a best friend that was diagnosed with GATA2 she is now going thru bad pain a mass in her stomach spot on her lung extreme weight loss an no energy sleeps all the time immune is 1. Something it’s aweful any advice
LikeLike
Oh dear, that sounds really difficult for your friend and for those who love her. GATA2 mutations seem to be quite unpredictable in how they affect some people.
However the medical knowledge regarding the effects of GATA2 and the best forms of treatment is steadily improving. She needs to keep in close contact with her doctor, making him/her aware of all of her symptoms, hopefully her doctor will liaise with those who are experts in treating people with GATA2 deficiencies, so that he/she can provide her with the best possible care.
LikeLike
Hi,
I have recently been diagnosed with MDS, caused by GATA2 deficiency. At the moment my symptoms are mild – constant cold/flu symptoms of varying degrees, warts/veruccas, molluscum contagiosum. There is barely any research/useful/comforting information online, I am 25 years old and my first doctors appointment was when I was 19 and I still feel like I don’t know enough. I am so sorry to read about Leah as it seems everything progressed far too quickly. I just wanted to comment to thank you for your blog as in a way I find it comforting that I am not alone with this illness that never seems to go away.
LikeLiked by 1 person
Hi Katie, thank you for saying hello. I’m sorry to hear that you aren’t well and I’m really sorry that you feel so alone with your diagnosis. GATA2 deficiency and all it entails is a relatively new diagnosis, most of the online information consists of research papers and these can be difficult to read and understand. I hope that you have a lovely hospital consultant and/or clinical nurse specialist like we had, who can answer some of your questions. You will be in my thoughts and prayers. Vicky
LikeLike
I’m so sorry to hear about your daughter, and thank you for Writing the blog. I was wondering if you have ever read about patients with GATA2 deficiency who have been diagnosed with acute lymphoblastic leukemia? I’ve only read of cases of AML. My 7 year old son was diagnosed with acute lympthoblastic leukemia (ALL) two years ago. I found it interesting that people with the deficiency can have non-cystic fibrosis bacterial lung infections. As my son had that when he was 10 months old for 8 months. I’ve always felt there is something wrong with his immune system. And I’m determined to figure it out. It’s always so frustrating that he is always treated to kill the cancer, but no one ever seems to care about why he got it in the first place. Any information would be helpful. Thank you.
LikeLiked by 1 person
Dear Sara, I’m so sorry to hear that your son has been so unwell and I hope that his ALL has responded well to treatment. I can certainly understand your wish to make sense of all that has been going on in your child’s body but from what I have read and heard I suspect that the GATA2 gene does not hold the clue. Well respected sites that describe the symptoms of GATA2 deficiency seem quite convinced that it is only AML that is associated with a GATA2 deficiency e.g.https://www.niaid.nih.gov/topics/gata2/Pages/default.aspx
However, the consultant who diagnosed Leah explained that we are at the cusp of a wave in terms of our understanding of the genetics of cancer. Perhaps as time goes on, the answers to your questions will become clearer. However keep asking those questions and I hope and pray that your son responds to treatment and experiences good health.
For a more academic understanding (but very general) of the genetics of cancer, check out this free six week online course from the University of Bath:
https://www.futurelearn.com/courses/inside-cancer
LikeLiked by 1 person